20 DBT Worksheets and Dialectical Behavior Therapy Skills
 Dialectical Behavior Therapy is an interestingly named treatment.
Dialectical Behavior Therapy is an interestingly named treatment.
If you’re as lost as I was when I first heard the term, then you’ve come to the right place. In this piece, you will learn what DBT is, how it works, and some of the most useful and applicable components of treatment.
Whether you are someone who is thinking about participating in Dialectical Behavior Therapy, a therapist who is looking for DBT worksheets to use with clients, or just a curious individual, read on to learn more about it.
Mindfulness is critical to DBT. Before you read on, we thought you might like to download our three Mindfulness Exercises for free. These science-based, comprehensive exercises will not only help you cultivate a sense of inner peace throughout your daily life but will also give you the tools to enhance the mindfulness of your clients, students or employees.
This Article Contains:
- What is Dialectical Behavior Therapy? A Definition
- About the Founder by Marsha Linehan
- DBT vs. CBT: How Do They Differ?
- 4 Essential DBT Skills & Techniques to Master
- 4 DBT Worksheets, Handout and Manuals (PDF)
- What Is The Diary Card All About?
- The 4 Best Books on DBT
- Treatment Methods Based on DBT and Emotion Regulation
- Certification Possibilities & Courses
- What is DBT’s Role in Mindfulness?
- A Take-Home Message
- References
What is Dialectical Behavior Therapy? A Definition.
Dialectical Behavior Therapy (DBT) is a type of cognitive-behavioral therapy that focuses on the psychosocial aspects of therapy, emphasizing the importance of a collaborative relationship, support for the client, and the development of skills for dealing with highly emotional situations (Psych Central, 2016).
DBT was created for the treatment of individuals struggling with suicidal thoughts but has matured into a treatment for a range of other conditions that involve dysfunctional emotional regulation. It is currently considered the “gold standard” for borderline personality disorder and has even been applied to the treatment of substance abuse and eating disorders (Linehan Institute, n.d.).
DBT is generally characterized by its two main components:
- Individual weekly therapy sessions;
- Weekly group therapy sessions.
Individual Weekly Therapy Sessions
These individual sessions are an opportunity for the therapist and client to address the issues and solutions that came up over the last week, with special attention paid to self-destructive or potentially self-harmful behaviors. These behaviors are targeted not only because they are inherently worrisome, but also because they can seriously disrupt the treatment process and undermine treatment goals.
Clients and therapists work as a team in these individual sessions, with the focus on learning and improving social and coping skills. They may also discuss more general issues relevant to improving the client’s quality of life, or more specific issues like post-traumatic stress disorder.
Weekly Group Therapy Sessions

These sessions are usually scheduled for two and a half hours and generally focus on developing skills from one of four skill areas:
- Interpersonal effectiveness;
- Distress tolerance/reality acceptance skills;
- Emotion regulation;
- Mindfulness skills.
Skill Modules
These four skill modules cover a wide range of useful skills that can be applied in daily life:
1. Interpersonal Effectiveness Module
The skills in this module are related to interacting with others, especially in difficult or potentially damaging situations.
These skills are intended to help clients function effectively when trying to change something (e.g., making a request) or in trying to resist changes (e.g., refusing a request). The intention is to aid the client in meeting their goals in each situation while avoiding any damage to the relationship or to the client’s self-respect (Psych Central, 2016).
2. Distress Tolerance Module
This module includes skills that are extremely important yet often overlooked: skills relating to accepting, tolerating, and learning from suffering.
Many other mental health treatment regimens focus on avoiding pain, changing difficult situations, or walking away from circumstances that cause suffering, but the distress tolerance skills taught through Dialectical Behavior Therapy focus on dealing with the pain and suffering that is inevitable to the human condition.
The distress tolerance module is split into four crisis survival strategies:
- Distracting;
- Self-soothing;
- Improving the moment;
- Thinking of pros and cons.
In addition, there are many skills that relate to accepting and tolerating the current situation, like radical acceptance and willingness vs. willfulness.
3. Emotion Regulation Module
Many clients who participate in DBT are struggling with personality or mood disorders and can benefit immensely from emotion regulation skills.
Some of these skills that can help clients deal with their emotions include:
- Identifying and labeling emotions;
- Identifying obstacles to changing emotions;
- Reducing vulnerability to “emotion mind;”
- Increasing positive emotional events;
- Increasing mindfulness to current emotions;
- Taking the opposite action;
- Applying distress tolerance techniques (Psych Central, 2016).
4. Mindfulness Module
Readers of this blog are likely already aware of the numerous mindfulness-related skills that can benefit them in their daily life.
These skills include “what” skills or skills that answer the question “What do I do to practice core mindfulness skills?” like observing, describing, and participating. There are also “how” skills or skills that answer the question “How do I practice core mindfulness skills?”, like non-judgment and practicing “One-mindfully” effectively.
Many of these mindfulness skills feed into skills from the other modules; for example, the nonjudgment encouraged in mindfulness is also encouraged in distress tolerance, and the observing and describing skills can be helpful in identifying and labeling emotions.
About the Founder Marsha Linehan

Dialectical Behavior Therapy was developed by Dr. Marsha Linehan.
She is a Professor of Psychology and adjunct Professor of Psychiatry and Behavioral Sciences at the University of Washington and Director of the Behavioral Research and Therapy Clinics, a research consortium that explores treatments for severely disordered and suicidal individuals (The Linehan Institute, n.d.).
Dr. Linehan is dedicated to promoting effective and accessible resources for the treatment of individuals who are struggling.
Dr. Linehan founded Behavioral Tech LLC, an institute focused on developing and sharing treatment tools for DBT training, consultation, and treatment. Behavioral Tech Research, Inc., was also established by Dr. Linehan in an effort to incorporate online and mobile technology into the successful practice of DBT.
Dr. Linehan approaches her scientific research and development from a perspective that is relatively uncommon in the sciences: one based in spirituality. She has trained with a number of spiritual leaders and influential thinkers, including a Zen master.
This may help explain her affinity for mindfulness, which grew to prominence through a collaboration of traditional Buddhist philosophy and the modern scientific paradigm (The Linehan Institute, n.d.).
DBT vs. CBT: How Do They Differ?

Of course, DBT is a type of CBT, so similarities are understandable. But DBT also has distinct features that set it apart from most CBT approaches.
DBT, like CBT, focuses on helping people address their dysfunctional thinking and behavior through modification of their thought patterns and, through changing their thoughts, their behavior as well. However, CBT is usually confined to a limited period of time and is often applied with one or two specific goals in mind.
On the other hand, DBT narrows the focus to psychosocial aspects of daily life. Many people have trouble with their thought and behavior patterns, but these issues are often at their most disruptive in the context of relationships with others. DBT was created to approach treatment from this angle, one that is often incorporated in general CBT but is not typically the main focus (Grohol, 2016).
This emphasis on relating to others is what explains the DBT-specific treatment component of group therapy sessions. The benefits of additional therapy to the treatment of severe emotion regulation dysfunction are clear, but it’s the group aspect that really helps explain its importance.
Adding group dynamics to the learning setting offers clients an opportunity to practice relational skills in a safe and supportive environment, a practice that has been shown to be extremely effective.
DBT also differs from general CBT in the use of clients’ history. Both incorporate the past in striving for a healthier future, but this discussion is not a focus of the therapy in DBT as it often is in CBT (Grohol, 2016). The perspective of DBT is that one can learn from their past, but that problems are inevitably rooted in current thoughts and behaviors, and the present is where these will be addressed.
4 Essential DBT Skills & Techniques to Master

We won’t go into all of them in detail, but these are the main skills and techniques applied in DBT.
Interpersonal Effective Skills
1) Objectiveness Effectiveness “DEAR MAN” Skills
- Describe;
- Express;
- Assert;
- Reinforce;
- Mindful;
- Appear confident;
- Negotiate.
2) Relationship Effectiveness “GIVE” Skills
- Gentle;
- Interested;
- Validate;
- Easy manner.
3) Self-Respect Effectiveness “FAST” Skills
- Fair;
- Apologies / no apologies;
- Stick to value;
- Truthful.
Distress Tolerance Skills
1) Crisis Survival “ACCEPTS” Skills
- Activities;
- Contributing;
- Comparisons;
- Emotions;
- Pushing away;
- Thoughts;
- Sensations.
2) Self-Soothing Skills
- Taste;
- Smell;
- See;
- Hear;
- Touch;
3) Improve the Moment “IMPROVE” Skills
- Imagery;
- Meaning;
- Prayer;
- Relaxation;
- One thing at a time;
- Vacation;
- Encouragement.
4) Pros and Cons / Accepting Reality Skills
- Willingness;
- Turning your mind;
- Radical acceptance.
Emotion Regulation Skills
1) Reducing Vulnerability Skills
- Treat physical illness;
- Eating;
- Altering drugs (only those prescribed by a doctor);
- Sleep;
- Exercise.
2) Build Mastery Skills
- Build positive experiences;
- Be mindful of current emotion;
- Opposite to emotion action.
Mindfulness Skills
1) “What” skills
- Observe;
- Describe;
- Participate.
2) “How” skills
- Non-judgmentally;
- One-mindfully;
- Effectively (Dietz, 2012).
As you can see, acronyms are front and center in DBT treatment, in part because it makes remembering these skills in important moments easier.
You may also notice that many of these skills are generally considered effective skills, rather than specific skills for specific problems. While Dialectical Behavior Therapy focuses on the treatment of severely distressed individuals, the means of working towards these goals are not mystical or mysterious. The methods of furthering treatment are grounded in common sense and the straightforward practice of skills.
In fact, these skills are so generally applicable that many of them have practical applications for everyone.
Mindfulness
Mindfulness is such a simple and beneficial practice that it’s hard to sum up the potential positive impacts in one section, let alone one article (but we gave it a shot anyway – see our piece on the benefits of mindfulness).
“Mindfulness can be described as simply living your life in the present instead of being stuck in the past or the future. Practicing mindfulness helps us become more aware of our thought patterns, our emotions, and how our thoughts and feelings affect our reactions to events” (Tartakovsky, 2015A).
If your mind has you jumping on the thought train (i.e., one thought leads to another, which often leads to a “should” thought, which can lead to judgment), try to detach yourself from the thought by telling yourself about the thought you are having (e.g., “There’s a thought about the errand I need to run after work”).
This can help you refocus on your current practice and remind yourself that you have thoughts, but you are not your thoughts (Tartakovsky, 2015A).
If you’re interested in learning more about how to practice mindfulness, check out our post on mindfulness exercises and techniques.
Reality Acceptance

Accepting reality is an effective antidote for a common problem in our society: struggling against the pain and suffering that is inherent to life as a human. DBT and Acceptance and Commitment Therapy (ACT) have this in common – both teach that accepting our reality, including the unpleasant aspects of it, is the only way to thrive.
This skill can be harder to practice and build than it seems since there are all sorts of sneaky ways we find to deny the reality of our situation.
These examples from Psych Central can shed some light on when we fight reality and how we can stop this tendency:
- You need to rush home, but you’re catching every red light. Instead of getting frustrated, you take a deep breath and tell yourself: “It is what it is. I’ll get home when I get there.”
- You need to fill up your car, but gas prices have skyrocketed. Again, you breathe deeply, and say to yourself: “There’s nothing I can do about it. I need gas. Getting angry isn’t going to help.”
- You have to walk to work because your car is in the shop. It’s not far, but it’s pouring. You take a deep breath and say: “It’s just rain. I’ll bring a towel, and I’ll dry off when I get to work” (Tartakovsky, 2015A).
The part-humorous, part-helpful Tumblr blog “Shit Borderlines Do” provides some steps towards practicing this skill in the moment:
- Observe that you are fighting the reality of your situation. Acknowledge that you are reacting to something that you cannot change;
- Remind yourself what the reality is, even if it’s difficult or upsetting;
- Consider the causes of the current reality and incorporate the skill of non-judgment to remind yourself that this is a random occurrence set in motion by a million other factors that are outside of your control;
- Accept this reality with your whole being, or your mind, body, and spirit. Pay attention to the bodily signs of fighting reality (e.g., posture, “fight-or-flight” response) as well as the spiritual signs (you may “know” that this is real, but you don’t “feel” like it’s real).
These steps are by no means exhaustive or required to accept reality, but they can be helpful in the moment.
Radical Acceptance
Dialectical Behavior Therapy’s radical acceptance technique can help in these situations.
Radical acceptance is simply acknowledging the reality of your circumstances instead of fighting it by thinking “This shouldn’t be happening” or “This isn’t fair.”
It can be difficult to accept pain, but fighting the reality of your pain only creates more pain, and this pain is optional. Instead of fighting pain, radical acceptance offers a way to accept it and address it.
In the words of psychotherapist Sheri Van Dijk:
“If you don’t like something, you first have to accept that it is the way it is before you can try to [change] it. If you’re not accepting something, you’ll be so busy fighting that reality that you don’t have the energy to put towards trying to change it” (Tartakovsky, 2015).
This explanation shows us that not only can radical acceptance help us accept the reality of things that we cannot change, it can also help us to realize what can be changed.
Non-judgmental Stance

Being non-judgmental means that you avoid assigning value to events and feelings.
Instead of facing a difficult situation and thinking “This is awful,” practicing non-judgment allows us to take a step back and realize that the value judgments we make are based on facts (the facts of what is happening) and the emotions we are feeling in reaction (Tartakovsky, 2015B).
For example, you may be stuck in accident-related traffic and thinking “People are such idiots.” If you make an effort to be nonjudgmental, this may translate to “I’m stuck at a standstill in traffic because of an accident up ahead. This makes me frustrated and upset.”
When you break a judgment down into a fact and your emotional reaction, you not only reduce the emotion(s) you are feeling, you can also be empowered to think about ways to solve the problem and make healthy decisions.
Say you are thinking about how selfish your significant other is being right now. Instead of stopping at “My partner is so selfish,” practicing non-judgment may lead to articulating the issue (“My partner is not helping me with this problem, and that makes me angry and disappointed”) and finding a way to solve it (“This is not a wise use of my time and energy. I will talk to my partner about how his/her unwillingness to help me with this problem makes me feel, and try to negotiate a solution with him/her”).
Handling emotional situations in this manner can not only help you reduce your emotional reaction and find smart solutions to problems, it can also improve your self-esteem and self-respect when you handle the issue in a way that makes you proud of yourself (Tartakovsky, 2015B).
4 DBT Worksheets, Handout, and Manuals (PDF)

This is where Dialectical Behavior Therapy worksheets, handouts, and manuals can prove to be extremely effective tools in building your skills and improving your ability to accept your situation, deal with difficulty, and solve problems.
We’ll go over some of the most popular and effective ones below.
DBT Interpersonal Effectiveness Skills
This handout lists and describes the interpersonal effectiveness skills we outlined earlier, and also provides useful tips to put these skills into practice.
For example, the section on objective effectiveness (the DEAR MAN skills) lists the following tips:
Describe
- Use clear and concrete terms to describe what you want;
- Don’t say: “Could you please clean?”;
- Do say: “Could you do the dishes before going to bed?”
Express
- Let others know how a situation makes you feel by clearly expressing your feelings;
- Don’t expect others to read your mind;
- Try using this line: “I feel ___ because ___.”
Assert
- Don’t beat around the bush—say what you need to say;
- Don’t say: “Oh, well, I don’t know if I can cook tonight or not;”
- Do say: “I won’t be able to cook because I’m working late.”
Reinforce
- Reward people who respond well, and reinforce why your desired outcome is positive;
- This can be as simple as a smile and a “thank you.”
Mindful
- Don’t forget the objective of the interaction;
- It can be easy to get sidetracked into harmful arguments and lose focus.
Appear
- Appear confident;
- Consider your posture, tone, eye contact, and body language.
Negotiate
- No one can have everything they want out of an interaction all the time;
- Be open to negotiation;
- Do say: “If you wash the dishes, I’ll put them away.”
The Wise Mind
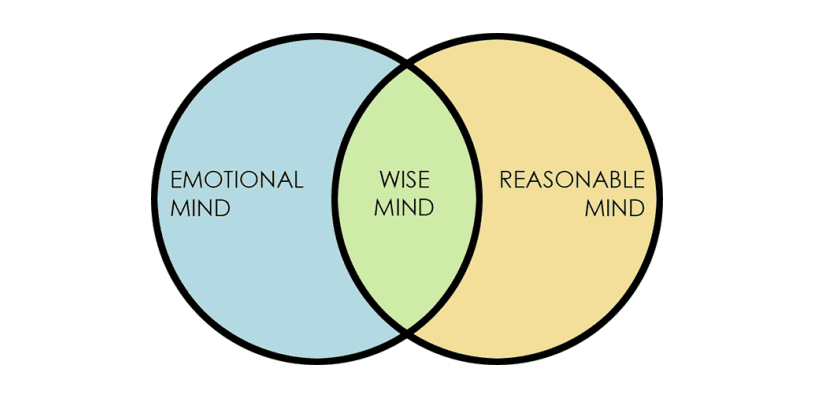
It is a balance between the two minds and is characterized by the ability to recognize and respect your feelings, but also respond to them in a rational manner.
The worksheet offers space to describe an experience that you have had with each of these three “minds” to further your understanding of the minds and how they have come into play in your life.
Function of Emotion Worksheet
The Function of Emotion Regulation worksheet helps you to identify the function of an emotional reaction you have had over the last week.
The worksheet moves through the following questions and steps:
- What was the prompting event?
- What was your interpretation?
- What was the emotion and intensity (0-100)?
Use the following to identify the function(s) of the emotion:
- Did the emotion communicate something to others or influence their behavior? If so, describe;
- Did the emotion organize or motivate you to do something? If so, describe;
- Did the emotion give you information, color your perception, or lead you to any conclusions? If so, describe.
These questions aid the individual in making the connections between a galvanizing event and the reaction s/he had to the event, as well as understanding how the emotional reaction impacts the self and others.
DBT Skills Training Manual: Second Edition
For a resource that can help you apply general DBT treatment, check out this manual from Dr. Linehan herself. It’s not free, but it is an extremely valuable resource for applying DBT with your clients.
This manual is separated into two parts: the first describes DBT and provides instructions on how to set up a treatment program and manage the problems that can arise, while the second gives detailed notes on teaching each DBT skill.
Check out the manual, buying options, and reviews from some very satisfied readers here.
What Is The Diary Card All About?

According to dbtselfhelp.com:
“You use the card to track your urges, moods, how you did or did not use DBT Skills, your feelings, and whatever else is helpful to you. You bring these cards with you to your DBT therapist every week to help you look for behavior patterns and triggers that occur in your life. Such information is invaluable to help you to help yourself live a life worth living.”
There are many possible layouts for a diary card (see here, here, and here), but they generally contain the same fields:
- Day/date of urge or behavior;
- Emotions felt;
- Actions taken or skills used (or not used);
- Triggers for the urges.
The diary card may also include space for a general rating for the day and any medications or substances used (legal or illegal).
The client is encouraged to fill out this card regularly and faithfully. While it is important that the client does so, they should know that no one is going to score them or judge them based on their diary card. It is not an assignment to be completed and graded, but a way for them to track their experience and evaluate their progression through DBT treatment and, hopefully, self-improvement.
Diary Card App
As with most problems or issues, technology is making an impact on how people keep diary cards.
If you hate to waste paper, don’t like getting ink on your hands, or just get tired of writing, there’s a diary card app that you can use instead.
Check out the app created by a licensed clinical psychologist here.
The 4 Best Books on DBT
If you’re interested in learning more about Dialectical Behavior Therapy, as a client, therapist, or just a curious person, there are several books available.
Listed below are some of the most popular and highly reviewed books on DBT out there, and they’re all available for purchase on Amazon.com:
1. The Dialectical Behavior Therapy Skills Workbook – Matthew McKay, Jeffrey C. Wood, and Jeffrey Brantley
It walks the reader through descriptions of DBT and how it can help, introductory exercises, and more advanced skill chapters. This can be an excellent resource for any individual considering DBT or for therapists to recommend to their clients.
Available on Amazon.
2. DBT Made Simple: A Step-by-Step Guide to Dialectical Behavior Therapy – Sheri Van Dijk
It includes a section on the theory and research behind DBT and how it grew from traditional CBT approaches, as well as strategies for working with clients, an explanation of the four skill modules, and several handouts, case examples, and some sample therapy dialogue.
Available on Amazon.
3. The Mindfulness Solution for Intense Emotions: Take Control of Borderline Personality Disorder with DBT – Cedar R. Koons and Marsha M. Linehan
It teaches readers about the seven powerful skills related to mindfulness and emotion regulation that can help people cope with a borderline personality disorder (BPD), post-traumatic stress disorder (PTSD), severe depression, and other emotion regulation problems.
Available on Amazon.
4. Calming the Emotional Storm: Using Dialectical Behavior Therapy Skills to Manage Your Emotions and Balance Your Life – Sheri Van Dijk
With a rating of over 4.5 out of 5 stars from nearly 50 customers, it sounds like the description is accurate.
Available on Amazon.
These books are an excellent start to learning about DBT and applying the skills in your clients’ lives, but if you’re looking for even more, visit this website to learn about other helpful books.
Treatment Methods Based on DBT and Emotion Regulation

- Understanding one’s emotions;
- Reducing emotional vulnerability;
- Decreasing emotional suffering (Bray, 2013B).
There are several ways to work toward these goals.
One of the websites we mentioned earlier, dbtselfhelp.com, offers an outline of how to build emotion regulation skills:
Interpreting Emotions
We all have emotions, but there is a theory that there are only a few basic emotions while the rest is interpretation and evaluation.
You can work on your skills related to interpreting emotions by completing a writing challenge described here.
Describing Emotions
Emotions involve action urges, prompts to perform certain behaviors. These urges are not part of the emotion but can feel like they are. There is often a prompting event, followed by interpretation, body changes in response to the emotions, and action urges.
This can lead to an effective or dysfunctional expression of emotions, which can have a wide range of consequences. To work on describing emotions, try to describe the qualities of your emotions and pay attention to things that may interfere, like secondary emotions that spring from the original emotion.
Follow this link for more information on describing emotions.
Function of Emotions
Emotions have three major functions in DBT:
- They communicate to and influence others;
- They organize and motivate action, and;
- They can be self-validating.
You can learn about the function of emotions by answering questions like “What are some examples of situations where your expressions of emotion were misread?” and “Can you think of some times when you misread the emotions of someone else?”
See this page for more information.
Reducing Vulnerability
We are all vulnerable to negative emotions, but we can build our skills related to reducing vulnerability. You can keep track of the factors that affect your physical and mental wellbeing, like your diet, any mood-altering drugs, sleep, and exercise.
Refer to these skills in the emotion regulation module for more information.
Paying Attention to Positives
Increasing positive emotions can be an effective method for dealing with difficult emotions. To build this skill, focus on the positive experiences you have throughout the day (short-term experiences) and the bigger, more impactful ones (long-term experiences).
Focus on building and maintaining positive relationships, and give mindfulness a try to savor positive experiences.
Letting Go of Painful Emotions
On the flipside of savoring the positive, letting go of the negative also has a place in emotion regulation. While accepting that pain happens is healthy, dwelling on negative emotions is dysfunctional.
Practice observing your emotions, describing and accepting them but not allowing yourself to be overwhelmed by them.
See this page for more information on letting go.
Opposite to Emotion Action
This technique is used to change painful emotions that are harmful rather than helpful. It is not about suppressing our emotions, but accepting the emotion and using it to take a different action.
To practice this technique, list some examples of when you have acted opposite to your current emotion. Describe a situation in which it is not appropriate to act opposite to your emotion to help you learn about the difference between each situation.
Check out this handout for more information.
What is Dialectical Behavior Therapy for adolescents (DBT)? – UC San Francisco
Certification Possibilities & Courses
Dialectical Behavior Therapy is a recognized treatment that is well supported by the evidence. There are many ways to learn about applying DBT, but getting certified is a great option. There are courses and online DBT training for both individuals interested in practicing DBT and for therapists and other mental health professionals who wish to apply DBT in their work.
For Therapists and Other Mental Health Professionals
Dr. Linehan’s Behavioral Tech Research Institute provides information on Dialectical Behavior Therapy certification for therapists. The certification is available through the DBT-Linehan Board of Certification and requires the following:
- A graduate degree in a mental health-related field from a regionally accredited institution of higher education;
- A mental health practitioner license;
- A minimum of 40 didactic training hours specific to DBT Clinical experience with DBT (at least three clients);
- DBT team experiences (at least 12 months of preparation and current participation on a DBT team);
- DBT skills knowledge/experience;
- You must have read the Skills Training Manual for Treating Borderline Personality Disorder by Marsha Linehan, completed all the homework assignments in the manual, and taught or participated in all modules of skill training;
- Successful pass of exam based on the Cognitive-Behavioral Treatment of Borderline Personality Disorder by Marsha Linehan;
- Letter of recommendation from your team leader;
- Work product demonstration (videotapes of three consecutive live therapy sessions);
- Mindfulness experience (at least one of the following: a mindfulness retreat, formal practice community participation, formally a student of a recognized Zen/contemplative teacher, or at least one formal training in mindfulness).
You can also become certified through the Dialectical Behavior Therapy National Certification and Accreditation Association (DBTNCAA). This allows you to list a specialized certification in DBT when you apply to Health Care Providers and HMO networks.
What is DBT’s Role in Mindfulness?

While DBT and mindfulness are not synonymous, they are certainly linked.
DBT is a therapy based on identifying, describing, and modifying thoughts and feelings. Mindfulness has clear applicability in this therapy, through its ability to help practitioners to become more aware of their feelings, thoughts, impulses, and behaviors (Bray, 2013A).
One description of the benefit of mindfulness in Dialectical Behavior Therapy is that it provides the individual with the ability to take control of the mind instead of having the mind control the individual.
Practicing mindfulness helps the individual in DBT to direct their attention to observing, describing, and participating in a nonjudgmental way, which enhances the individual’s skills and leads to improved ability to focus on the positive, let go of the negative, and regulate emotions.
As we’ve said before, mindfulness is an extremely useful skill for individuals dealing with difficult emotions or situations, but it can be an even more effective tool for people struggling with a diagnosis.
A Take-Home Message
The intention of this piece was to provide an overview of Dialectical Behavior Therapy and outline the skills and tools that can help you or your clients to address emotion regulation issues. I hope it has met this goal, and that you know much more about Dialectical Behavior Therapy than you did when you started!
I hope you also keep in mind that the skills involved in DBT are applicable for those that are not suffering from a diagnosed mental health issue as well. Skills like mindfulness, focusing on the positive, letting go of the negative, and accepting the reality of your situation have clear benefits for everyone, not just those who are in the midst of suffering.
Have you tried DBT? Have you applied DBT with your clients? As always, please let us know about your experiences in the comments.
Thanks for reading!
We hope you enjoyed reading this article. Don’t forget to download our three Mindfulness Exercises for free.
- Bray, S. (2013A). Core mindfulness in Dialectical Behavior Therapy. GoodTherapy. Retrieved from http://www.goodtherapy.org/blog/core-mindfulness-dialectical-behavior-therapy-0215134
- Bray, S. (2013B). Emotion regulation in Dialectical Behavior Therapy. GoodTherapy. Retrieved from www.goodtherapy.org/blog/emotion-regulation-dialectical-behavior-therapy-dbt-0318135
- Dietz, L. (2012). DBT skills list. DBT Self Help. Retrieved from www.dbtselfhelp.com/html/dbt_skills_list.html
- Grohol, J. (2016). What’s the difference Between CBT and DBT? Psych Central. Retrieved from https://psychcentral.com/lib/whats-the-difference-between-cbt-and-dbt/ Linehan Institute
- Psych Central. (2016). An overview of Dialectical Behavior Therapy. Psych Central. Retrieved from https://psychcentral.com/lib/an-overview-of-dialectical-behavior-therapy/
- Tartakovsky, M. (2015A). 3 DBT skills everyone can benefit from. Psych Central. Retrieved from https://psychcentral.com/blog/archives/2015/08/28/3-dbt-skills-everyone-can-benefit-from/
- Tartakovsky, M. (2015B). What it really means to practice radical acceptance. Psych Central. Retrieved from https://psychcentral.com/blog/archives/2015/10/04/what-it-really-means-to-practice-radical-acceptance/
- The Linehan Institute. (n.d.). Linehan Institute. Retrieved from http://www.linehaninstitute.org/about-Linehan.php
Let us know your thoughts
Read other articles by their category
- Body & Brain (49)
- Coaching & Application (57)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (24)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (20)
- Mindfulness (45)
- Motivation & Goals (45)
- Optimism & Mindset (34)
- Positive CBT (29)
- Positive Communication (20)
- Positive Education (47)
- Positive Emotions (32)
- Positive Leadership (18)
- Positive Parenting (4)
- Positive Psychology (33)
- Positive Workplace (37)
- Productivity (17)
- Relationships (46)
- Resilience & Coping (36)
- Self Awareness (21)
- Self Esteem (38)
- Strengths & Virtues (32)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)



What our readers think
I appreciate you giving this information.
In our online treatment, dialectical behavioral therapy is used. It works incredibly well for depression, substance abuse, and borderline personality disorder. Even the most serious cases respond very well to DBT, and we treat a wide range of clients.
I’ve been looking for this info!!! DBT saved my life and I believe EVERYONE could benefit from it. The reason I’ve been searching is for my boys. I never meant to pass that part of me to any of my children but I see it in them. I’m trying for them to avoid the wrong roads I took. I barely escaped the darkness. I couldn’t bare to see them in that place. So ty!! I can’t say it enough.
I have recently completed a DBT group therapy course which I found extremely helpful in managing my BPD and PTSD.
I would love to teach these skills to others worldwide, is it a requirement that you have a certain level of certification to teach cbt/dbt and if so what qualifications are required to go on to teach these skills to others online?
I believe I have enough personal experience, understanding and now knowledge of the skills and mental illness, but am confused on the law of teaching these skills without official certification, or even if that’s a must?
Please help
Hi Sonja,
That’s great your experience was so helpful for you! To teach CBT and DBT skills to support people with mental illnesses, you need to become a licensed therapist or psychologist. This requires that you complete a master’s qualification. You can learn more about the process in our dedicated blog post: https://positivepsychology.com/how-to-become-a-therapist/
Hope this helps!
– Nicole | Community Manager
I have the same question. I work in mental health as a life coach and yoga instructior. I do not want to teach the program. My intention is to use the “My life Vision” worksheet and the wise mind model. What is the legal implications? I would sight the source while being clear on my role and title. The client would be provided resources for a licensed therapist.
This is outstanding!!!!!!
Just curious, you mention in the section – Working with Primary and Secondary Emotions
While – “this webpage” but then there is no link to the webpage the article is referencing. I am wondering if you would direct me to the webpage please for further reference.
As well, in the following paragraph on Emotion Regulation, again you mention “this worksheet” but don’t link a worksheet.
Are you able to reference these for follow-up, please and thank you?
Hi Heather,
Thank you so much for being so observant and bringing this to our attention.
These links went to other websites, which may have restructured their content and caused dead links on our side. I have unfortunately not been able to trace the original worksheets discussed, but have amended our copy to prevent any further confusion.
Apologies for not being able to help you further.
Regards,
Annelé
I wish DBT was more available in standard mental health services.
In the UK, it’s thin on the ground.
BPD is prolific and causes so much suffering. Yet still much ignorance and stigma remains.
I hate the way so many blame and shame such lonely and fragile people.
We want love, but are terrified of our vulnerability being abused.
I wish I could’ve got this treatment. My partners would not have had to put up with so much, maybe.
Damaged people damage people.
Hi Josh,
Thank you for sharing your thoughts on the availability of Dialectical Behavior Therapy (DBT) and the challenges faced by individuals with Borderline Personality Disorder (BPD). It is indeed disheartening to hear that access to this valuable treatment is limited in the UK and that stigma continues to surround BPD.
The importance of raising awareness about mental health conditions and advocating for better access to evidence-based treatments, such as DBT, cannot be overstated. It is essential to create a more understanding and compassionate society that supports individuals with mental health challenges instead of perpetuating shame and blame.
I encourage you to check out Psychology Today! It has a great directory you can use to find therapists in your local area. Usually, the therapists provide a summary in their profile with their areas of expertise and types of issues they are used to working with.
Please know that your voice matters and your experiences can contribute to raising awareness, challenging stigmas, and ultimately improving mental health care for those who need it most.
Warm regards,
Julia | Community Manager
I have been waiting a very long time for DBT therapy for diagnosed Borderline Personality Disorder, being unable to work for 20 months now. I have finally been assigned a place but am unable to purchase DBT Skills Training Handouts and Worksheets Second Edition. Seeking help from so many places, I can’t even find a Microsoft Word version of the worksheets that I can complete online in order to participate in the group therapy. As a result, I cannot have the therapy I desperately need. I know this is a long shot, but does anyone have a version in Word (or Open.Office) that they can send to me?? Otherwise, I will continue to suffer as the NHS has taken so long to help me with a condition I have had for decades, together with my depression and anxiety. Thanking you in advance.
Hi Dawn,
I’m sorry to hear you’ve had so much trouble receiving support. Please let me know which specific worksheet(s) you are trying to open, and I will let you know the best way to do so with free software.
– Nicole | Community Manager
Thank you for providing this information.
This sums up the group therapy session I have just graduated from! Modalities were based from Marsha’s core theories; it is alot of skills to practice.
Courtney, everything you wrote on this page IS TRUE, well written for any level audience. Well done.
Radical Acceptance, and Emotional identification is THE HARDEST part of BPD and DBT. I find it hard now to identify why I am in an “emotional crisis”, since I want to “Name it, to Tame it”. I really can’t identify why I become so deeply emotional (rage, crying, worthless…) but the emotions are EXTREME. I can’t identify what I was so emotional about, why I became so emotional in the first place ONCE I GET CAUGHT IN “THE DARK HOLE” as my husband refers to my “emotional crises”.
Just thought I would share my own personal experience; FYI I am an ongoing work in progress. Still have many ups and downs; however I can reflect on these events (usually AFTER the fact, but LIVE AND LEARN).
Super frustrting that it says “We hope you enjoyed reading this article. Don’t forget to download our 3 Mindfulness Exercises for free.” but you enter your information and then it tells you it cost $27.00. Why the false advertising…why say free just to get another person email to spam?
Hi Emily,
My apologies! Please try visiting this link to access the free downloads. The three exercises are definitely free! But if there’s a link in the text that tries to point you toward a paid resources, please let us know where it is so we can correct this 🙂
– Nicole | Community Manager