What is Teletherapy & The Benefits of Online Therapy
 For most people, we understand the benefits and sometimes the necessity of seeking out therapy. It can be a rewarding and valuable experience, helping us to overcome challenges and barriers in life we might not be able to face on our own.
For most people, we understand the benefits and sometimes the necessity of seeking out therapy. It can be a rewarding and valuable experience, helping us to overcome challenges and barriers in life we might not be able to face on our own.
Unfortunately, seeking out therapy is still something many people find difficult for several reasons. Whether it’s the lingering social stigma of needing support with our mental health or simply finding the time and capacity to sit down with a therapist.
Introducing teletherapy.
In our increasingly digitally connected world, we’re finding new ways to connect. Therapy is yet another area that has caught on to the power of digital connection and is already using it to help more people access the support they need.
Before you continue, we thought you might like to download our three Positive Psychology Exercises for free. These science-based exercises will explore fundamental aspects of positive psychology including strengths, values, and self-compassion, and will give you the tools to enhance the wellbeing of your clients, students, or employees.
This Article Contains:
- What is Teletherapy?
- How Do Online Therapy Sessions Work?
- Blended Care Approaches to Teletherapy Using Quenza
- Who is Teletherapy For?
- Are Teletherapy Sessions Private?
- Is Teletherapy as Effective as Face to Face Therapy?
- 4 Benefits of Teletherapy for Patients
- 4 Benefits of Teletherapy for Therapists
- 3 Online Therapy Software Platforms to Use
- A Take-Home Message
- References
What is Teletherapy?
While it has grown in availability over the last few years, teletherapy has been around since the 1990s in the United States and is considered a highly effective method for therapy delivery.
Goode and Shinkle (2019) created the following definition of teletherapy:
“Teletherapy is the online delivery of speech, occupational, and mental health therapy services via high-resolution, live video conferencing.”
Teletherapy, also known as online therapy, e-therapy, or video therapy, is therapy delivered through a virtual platform via a computer. If you’ve ever used FaceTime or Skype, it’s essentially the same thing – except more secure and with a qualified therapist or counselor at the other end instead of a distant friend or relative.
Where time zones or connectivity issues make live appointments inconvenient, teletherapy can also involve the use of time-delayed interventions and interactions. This enables patients to receive science-based treatments through video recordings, audio files, and more.
How Do Online Therapy Sessions Work?
Teletherapy sessions work much the same way as traditional therapy sessions with only one significant difference – the therapist and the client are not in the same room.
Many treatments, such as cognitive behavioral therapy (CBT) and mindfulness interventions, translate well into a digital format despite the therapist and client not being co-located. However, the means through which these interventions are carried out will differ depending on whether they are delivered through a synchronous or asynchronous mode.
Synchronous Teletherapy
In the case of synchronous teletherapy, sessions are scheduled at an appropriate and suitable time and day for each party, who then log-in via an agreed, secure video platform. The therapist and client can see and hear each other in real-time during the session via the use of webcams and headsets.
Through this virtual environment, they can interact with each other, and the therapist uses the same traditional techniques and activities they would use in a face-to-face therapy session (Goode and Shinkle, 2019).
As with face-to-face therapy, a client may only seek out the therapist for one session to deal with a current life situation, or they may agree to on-going sessions.
Asynchronous Teletherapy
With asynchronous teletherapy, clients are free to engage with interventions or learning materials at a pace that suits them – or they may follow a personalized treatment plan that they have collaborated on with their therapist.
Together, synchronous and time-delayed therapy might combine in a blended care approach to treat a wide range of conditions as a type of supplement to real-time meetings.
For example, the therapist may assign a client homework or an assessment to complete before their next in-person session. Alternatively, the therapist might encourage the client to engage with various multimedia activities between sessions, such as guided audio meditations or psychoeducational content in a video format using an online blended care platform.
Blended Care Approaches to Teletherapy Using Quenza
Quenza is a digital tool designed to help therapists and other helping professionals design and share digitized psychoeducational activities with their clients.
These activities can take the form of assessments, questionnaires, reflection exercises, audio-visual lessons, and more.
Once received, clients can complete the activities at their convenience (asynchronously) on their computer or using an Apple or Android device.
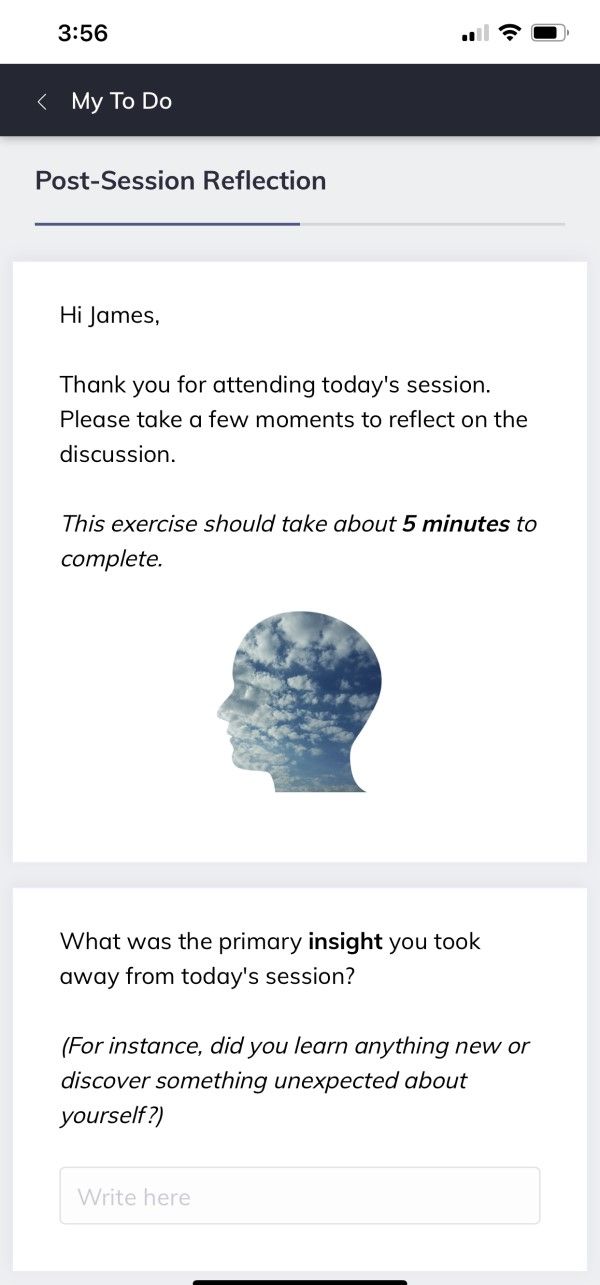
As an example (pictured here), the therapist has designed a reflection exercise in Quenza for the client to complete following their real-time (synchronous) therapy session conducted earlier that day.
Other examples of a blended care approach to teletherapy might be if the therapist were to invite their client to complete self-paced educational modules based on the aims of the therapy, such as on topics like cognitive restructuring or goal-setting.
Using Quenza, the therapist may then combine these modules into a unified pathway for the client to complete over several weeks, with automatically scheduled reminders for the client and deadlines that both the therapist and client can track via Quenza’s smartphone or desktop app.
This is just a few examples of how therapists might leverage a platform like Quenza as part of a blended approach to conducting teletherapy.
Who is Teletherapy For?
Teletherapy is beneficial for a range of people, for a diverse set of circumstances or experiences, including speech therapy, occupational therapy, and mental health therapy.
It has been used for regular one-to-one therapy sessions but also used in group therapy sessions to support aging individuals diagnosed with HIV (Heckman et al., 2014). Another way teletherapy has been used has been in the delivery of behavioral training to caregivers of young people with attention deficit hyperactivity disorder (Tse et al., 2015).
It is worth noting that teletherapy will not prove beneficial for all individuals in all circumstances. Many therapists recommend this as the first step towards therapy, especially for those seeking it for the first time and encourage participants to have open conversations with their therapist over whether this is the best pathway of support for them (Novotney, 2017).
Are Teletherapy Sessions Private?
Therapists are ethically and legally bound by privacy laws to not share details about their teletherapy sessions with third parties, just as with face-to-face sessions. Therapists must ensure they are in a private and secure room before engaging in any teletherapy sessions. Sessions should not be recorded or shared, unless with explicit agreement from the patient.
From the patient end, it is also down to them to ensure they conduct their end of the session in an equally private area to ensure their confidentiality.
Some therapists have argued that teletherapy is more private than traditional face-to-face sessions, where patients who know each other have the potential to bump into each other on the premises where therapy takes place.
Security compliance for teletherapy technologies
First, any technologies must meet the requirements of the 1996 Health Insurance Portability and Accountability Act (HIPAA).
In other words, they must be HIPAA Compliant. To be compliant with this legislation means that the technology provider has procedures in place to ensure data privacy and safeguarding of clients’ medical information and private information.
The European Union’s (EU) General Data Protection Regulation (GDPR) imposes similar standards for security and safeguarding of patient information, only with a focus on protecting European rather than US citizens’ information.
The earlier example of Quenza is one such platform that meets these data protection standards, ensuring that all interactions between therapists and their clients are secure thanks to personal PIN codes and 128-bit encryption. However, be wary that not all blended care platforms take these measures.
In sum, if you are a therapist interested in conducting teletherapy, take care to meet your legal and ethical obligations by ensuring that any technologies you use meet the security standards and regulations applicable to you and your client’s location.
Is Teletherapy as Effective as Face to Face Therapy?
How effective teletherapy is, really depends on the individual and their reasons for seeking therapy. Since it first began to be used as a treatment method more than 20 years ago, psychological research has explored the different ways teletherapy, or telepsychology, has been used, and its effectiveness.
Overall the research does support that teletherapy is just as effective as traditional face-to-face therapy for a range of circumstances.
A few key studies include:
- Wagner, Horn, and Maercker (2013) explored the benefits of teletherapy for supporting patients diagnosed with depression. Sixty-two patients were randomly assigned to two groups – one receiving teletherapy and the other receiving more traditional face-to-face therapy. The patients received eight sessions each, and at the end of their sessions, the group who received teletherapy showed a slightly higher percentage of reporting fewer depressive thoughts and feelings. After three months, the teletherapy group continued to report a decrease in depressive thoughts and feelings, compared to those treated traditionally who reported a minimal decrease.
- Acierno et al. (2014) studied the benefits of teletherapy for use in therapy with veterans experiencing PTSD. They worked with 132 veterans, asking them to complete a scale to measure PTSD and then randomly assigned them to one of two groups to receive 10-12 sessions of either face-to-face therapy or teletherapy. After three months and six months, respectively, the participants were asked to complete the PTSD scales again. At both points, the researchers found that those who were treated via teletherapy showed similar improvement to those treated face-to-face.
- Mitchel et al. (2008) worked with trained therapists to see if teletherapy could be effective with the treatment of patients experiencing bulimia nervosa. One hundred twenty-eight adults diagnosed with bulimia nervosa took part in the study and were randomly assigned to receive therapy either face-to-face or via teletherapy. Participants were asked to report if they were still participating in bingeing and purging behaviors after the initial sessions ended, three months later and twelve months later. The researchers found extremely minimal differences in recovery between the two groups.
Research to date shows very promising effectiveness for teletherapy, however many therapists stress that one of the critical components for successful therapy is the relationship between patient and therapist, and in-person connections can be vital for successful treatment. For individuals who experience difficulty forming relationships or struggle with social interaction, traditional face-to-face therapy could be more beneficial in overcoming these challenges.
4 Benefits of Teletherapy for Patients
Aside from its equal effectiveness as a therapy treatment, there are many other benefits to teletherapy for patients seeking it out. A few notable ones include:
1. Accessible to more people
For individuals living in rural communities, living with a disability that makes travel difficult, or those who are just unsure about trying therapy for the first time, teletherapy is a highly beneficial option. Teletherapy removes many of the barriers – physical, emotional, or mental – towards seeking out therapy and makes it accessible for more people.
Research has found that those who participate in teletherapy are also more likely to seek out face-to-face therapy as a result of a positive experience (Jones et al., 2014).
2. Offers greater flexibility
It’s easy to put off attending therapy when sessions are offered during limited office hours. For many people who already have a lot of commitments to juggle, seeking out this form of support can easily be bumped down the priority list. When a therapist can be readily available at a time that suits the patient, it offers greater flexibility and could even encourage more people to seek the right support when they need it most.
3. Reduced wait times
It might seem like a small benefit, but increased flexibility also means reduced waiting times for patients wanting to speak with a therapist urgently or for the first time. It can take a lot of courage making an appointment for therapy, and the less time someone has to wait, the more likely it will be they’ll follow through and get the help they need.
Taking time off from work to battle traffic while going to the therapist, wasting even more time in the waiting room, having the session, and then battling traffic to return to work, is also a huge deterrent to many. Being able to brew a quick coffee, step into a private room for the scheduled therapy session, and ready to return fairly soon to ‘work-mode’ is a much more viable solution for many office workers.
4. Creates a safer environment
That feeling of anxiety many experience when sitting in the waiting room of the dentist or doctor surgery? It’s the same anxiety experienced when waiting for a therapy session. The process of going to a new environment to meet with a therapist can be a stressful one. Teletherapy alleviates this stress by allowing patients to familiarise themselves with the process in the comfort of their own home.
4 Benefits of Teletherapy for Therapists
Just as teletherapy has benefits for the patients that use it, it also has benefits for the therapists that deliver it. A few of these include:
1. Offers greater flexibility and work-life balance
As with patients, the ability to work from the security of a home office or private therapy room offers therapists greater flexibility and availability to their patients. For therapists with multiple other life commitments, this flexible can make a huge difference in finding a positive work-life balance.
2. Lowers overheads for delivering therapy
With teletherapy, the therapist can deliver from any location that works for them, so a private home office works well. By removing the need for an external office location, therapists can significantly reduce their overhead financial costs, meaning they can focus more on professional development and patient support.
3. Offers a greater sense of safety
Therapists often take a risk when taking on new patients. People can react and behave in unexpected ways when working through the therapeutical process, and sometimes this can present itself in negative or even aggressive ways. For therapists working with new clients or clients with pre-diagnosed severe mental illness, teletherapy can allow them a safe distance to get to know the patient before moving to face-to-face therapy if deemed necessary.
4. Opens up new opportunities and areas of specialism
Teletherapy also has the benefit of offering therapists the ability to work with new patients, anywhere in the world. This can help them find not only new patients but patients they might not otherwise get the opportunity to support and engage with. This could include patients in the prison service, remote schools or communities, or patients restricted to hospitals.
Cost of starting a home teletherapy practice
3 Online Therapy Software Platforms to Use
Whether you’re a solo practitioner or part of a large organization providing teletherapy services, there are many useful digital technologies on the market to support any sized practice. Many of these technologies are also very reasonably priced.
When selecting a teletherapy software for your business, it is not only critical to ensure that the platform is HIPAA and/or GDPR compliant, but ensure it serves your specific business needs (e.g., secure video conferencing capabilities, the development and distribution of psychoeducational materials).
Therefore, we recommend you begin by explicitly evaluating what your business needs from an effective teletherapy platform, and any gaps or challenges in your current workflow.
Once you’ve done that, look at our round-up of three top-recommended teletherapy platforms and see if any meet these needs.
1. Quenza

We’ve already explored a couple of this platform’s functions in our discussion above, including its usefulness for digitally sharing psychoeducational activities with clients and enabling clients to complete these activities on their personal devices.
Other features worth noting are the platform’s intuitive drag-and-drop activity builder, which is the key tool enabling therapists to craft customized assessments, questionnaires, lessons, and other materials, tailored to their clients’ needs.
Quenza users also have the option to draw from the platform’s ever-expanding library of pre-loaded activities, all of which are based on science-backed positive psychology research.
Once designed or selected, therapists can choose to combine activities into a pathway, enabling them to craft sequences of educational or development materials that their clients can complete according to a predetermined schedule.
Further, the therapist can easily track how their clients are progressing through their activities from the platform’s dashboard and send push notification reminders to clients’ devices, reminding them to complete any overdue activities.
In sum, the platform functions as a useful tool for collating and sharing digital materials as part of an asynchronous, blended care approach to running a teletherapy practice.
If you’re interested in learning more, the platform currently offers a 30-day trial for just $1 to let you try Quenza and all its features for yourself.
2. Wecounsel.com
Wecounsel.com is a platform that caters to supporting behavioral health therapy. The platform is completely HIPAA compliant and ranks highly for its encryption ranking that also exceeds expected standards. It offers variable pricing plans, depending on the number of users and desired functionality.
3. Thera-link.com
Thera-link.com is a prevalent platform and was developed specifically for use within the mental health field by two therapists, with support from a technology expert. Thera-link.com seeks to be the one-stop platform therapists need when coordinating teletherapy and includes features such as session invitations, calendar management, invoicing, and payment. It is also entirely HIPAA compliant.
A Take-Home Message
I hope after reading this article, you’ll have a clearer idea of teletherapy; its benefits, and just how effective it can be for many people. There seems to be a false opinion that teletherapy isn’t as good as traditional face-to-face therapy, but in our digital world, it seems it can be a very positive solution for many people.
If there’s one thing I’d like you to take away from reading this, it’s that while the research is overwhelmingly in favor of teletherapy, it isn’t a one-size-fits-all method. Therapy is a deeply personal and individualized process, and what works for one won’t always work for another.
Have you had any experience with teletherapy? If you feel comfortable sharing, I’d love to hear about it in the comments section below.
We hope you enjoyed reading this article. Don’t forget to download our three Positive Psychology Exercises for free.
- Acierno, R., Knapp, R., Tuerk, P., Gilmore, A. K., Lejuez, C., Ruggiero, K., et al. (2017). A non-inferiority trial of Prolonged Exposure for posttraumatic stress disorder: In-person versus home-based telehealth. Behaviour Research and Therapy, 89.
- Goode, H. and Shinkle, E. (2019). What is Teletherapy? A Helpful and Definitive Guide. Retrieved from: https://globalteletherapy.com/what-is-teletherapy/
- Heckman, B. D., Lovejoy, T. I., Heckman, T. G., Anderson, T., Grimes, T., Sutton, M., et al. (2014). The moderating role of sexual identity in group teletherapy for adults aging with HIV. Behav Med, 40(3).
- Jones, M., Kass, A. E., Trockel, M., Glass, A. I., Wilfley, D. E., and Taylor, C. B. (2014). A Population-Wide Screening and Tailored Intervention Platform for Eating Disorders on College Campuses: The Healthy Body Image Program.
- Mitchel, J. E., Crosby, R. D., Wonderlich, S. A., Crow, S., Lancaster, K., Simonich, H., Swan-Kremeier, L., Lynse, C., and Myers, T. C. (2008). A randomized trial comparing the efficacy of cognitive-behavioral therapy for bulimia nervosa delivered via telemedicine versus face-to-face.
- Novotney, A. (2017). A Growing Wave of Online Therapy. Retrieved from: https://www.apa.org/monitor/2017/02/online-therapy
- Tse, Y. J., McCarty, C. A., Stoep, A. V., and Myers, K. M. (2015). Teletherapy Delivery of Caregiver Behavior Training for Children with Attention-Deficit Hyperactivity Disorder. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4458734/
- Wagner, B., Horn, A. B., and Maercker, A. (2013). Internet-based versus face-to-face cognitive-behavioral intervention for depression: A randomized controlled non-inferiority trial. Journal of Affective Disorders, 2013.
Let us know your thoughts
Read other articles by their category
- Body & Brain (49)
- Coaching & Application (57)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (24)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (20)
- Mindfulness (45)
- Motivation & Goals (45)
- Optimism & Mindset (34)
- Positive CBT (28)
- Positive Communication (20)
- Positive Education (47)
- Positive Emotions (32)
- Positive Leadership (18)
- Positive Parenting (4)
- Positive Psychology (33)
- Positive Workplace (37)
- Productivity (17)
- Relationships (46)
- Resilience & Coping (36)
- Self Awareness (21)
- Self Esteem (38)
- Strengths & Virtues (32)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)



What our readers think
Aloha… Ive been trying to reset my password but i get no reset email…?
Hi John,
Are you still experiencing this issue? If so, please email info@positivepsychology.com and our wonderful Customer Support team will help you right away 🙂
All the best,
-Caroline | Community Manager
You made a good point that accessibility is one of the key advantages of video therapy. My friend has been having a hard time dealing with her anxiety because she lives a lone in the middle of a pandemic that requires self-quarantining. It’s great to know that she can still have access to a therapist in case she really needs one within the comfort of her home.
https://neweratherapynow.com/video-therapy
Good afternoon! Where I can get a seminar or CE. Was so useful for me.